# Melasma (기미)
---
## 1. Definition
- **Melasma (기미)** is an **acquired hyperpigmentation disorder**, characterized by symmetric, irregular, brown-to-gray macules and patches.
- Typically appears on **sun-exposed areas**: face (malar, forehead, upper lip, nose, chin), and sometimes forearms.
- Chronic, relapsing, and strongly influenced by hormonal and environmental factors.
---
## 2. Epidemiology & Prevalence
- Common in women of reproductive age, especially **20–40 years**.
- Strong prevalence in darker phototypes (Fitzpatrick III–V).
- Female:male ratio ~9:1.
- More common in Asian, Hispanic, and Middle Eastern populations.
- Incidence increases during pregnancy (“mask of pregnancy”).
---
## 3. Pathophysiology
### A. Cellular and Molecular Basis
- **Melanocyte hyperactivity** (not hyperplasia): melanocytes produce more melanin.
- **Melanin deposition** in epidermis, dermis, or both.
- Key drivers:
- **UV radiation** → upregulates melanogenesis via melanocortin-1 receptor and α-MSH.
- **Hormones** → estrogen and progesterone increase melanocyte activity.
- **Genetic predisposition**.
### B. Pigment Distribution Types
- **Epidermal Melasma**: melanin in basal and suprabasal keratinocytes → brown, more responsive to treatment.
- **Dermal Melasma**: melanophages in dermis → blue-gray, resistant to therapy.
- **Mixed**: combination of both, most common.
### C. Vascular and Inflammatory Contributions
- Increased dermal vascularity may play a role.
- Disrupted basement membrane may allow melanin leakage into dermis.
---
## 4. Clinical Features
- **Presentation**:
- Symmetrical, irregular hyperpigmented patches.
- Face: centrofacial (forehead, nose, upper lip, chin), malar, mandibular.
- **Wood’s lamp examination**:
- Epidermal melasma → pigment enhancement.
- Dermal melasma → no enhancement.
- **Dermoscopic features**:
- Brown reticular network (epidermal).
- Bluish-gray granules (dermal).
- Mixed patterns common.
---
## 5. Histopathology
- Epidermal: basal hyperpigmentation, elongated rete ridges.
- Dermal: dermal melanophages, solar elastosis.
- Often accompanied by **increased vascularity**.
---
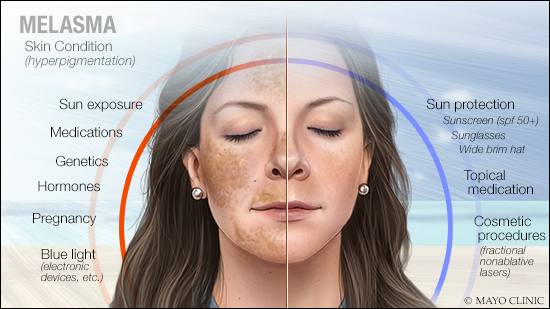
## 6. Risk Factors
- UV exposure.
- Pregnancy, oral contraceptives, HRT.
- Genetic predisposition (family history).
- Thyroid disease associations (controversial).
- Medications (e.g., phenytoin).
---
## 7. Management
### A. General Principles
- **Chronic and relapsing** → requires long-term control, not cure.
- Sun protection is cornerstone.
### B. First-line: Topical Agents
- **Hydroquinone** (HQ, 2–4%) → gold standard, inhibits tyrosinase.
- **Triple combination cream** (HQ + tretinoin + corticosteroid).
- **Alternative depigmenting agents**: azelaic acid, kojic acid, arbutin, tranexamic acid.
### C. Procedures
- **Chemical peels**: glycolic acid, salicylic acid (superficial).
- **Lasers/light therapy**:
- Low-fluence Q-switched Nd:YAG (1064 nm, “laser toning”).
- Fractional lasers.
- Risks: rebound hyperpigmentation, PIH, especially in darker skin.
- **Microneedling + tranexamic acid**: emerging therapy.
### D. Systemic Agents
- **Oral tranexamic acid** (off-label): reduces melanogenesis via plasmin inhibition.
- Caution: thromboembolic risk.
---
## 8. Prognosis & Patient Counseling
- Chronic, often recurs with UV or hormonal triggers.
- Requires **lifelong photoprotection**.
- Set realistic expectations: “Improvement and control” rather than complete cure.
---
## 9. Clinical Pearls
1. Melasma (기미) = melanocyte hyperactivity, not proliferation.
2. Epidermal type responds best to topical/laser; dermal type resistant.
3. Strict sun protection = most effective long-term therapy.
4. Oral tranexamic acid is promising but not without risk.
5. Always differentiate from post-inflammatory hyperpigmentation (PIH), drug-induced pigmentation, and lentigines.
Melasma (기미) is a chronic, hormonally and UV-driven acquired hyperpigmentation disorder. Histologically, it is due to melanocyte hyperactivity, with melanin deposition in epidermis and/or dermis. Clinically, it presents as symmetrical brown patches on sun-exposed skin. Management requires multimodal therapy (sun protection, topical agents, procedural treatments), with realistic counseling due to its relapsing nature.