### Date : 2025-07-26 15:44
### Topic : 2.3 Scalp Disorders Associated with Hair Loss
----
## 2.3 Scalp Disorders Associated with Hair Loss
Scalp disorders frequently accompany or cause hair loss. Recognizing, diagnosing, and appropriately treating these conditions are essential for effective management of alopecia.
We'll examine in detail:
- Seborrheic Dermatitis
- Psoriasis of the Scalp
- Fungal Infections (Tinea Capitis)
- Folliculitis and Eczema of the Scalp
---
## 1. Seborrheic Dermatitis
### Definition and Pathogenesis:
Seborrheic dermatitis is a chronic, inflammatory skin disorder primarily affecting sebaceous-rich areas. It is associated with increased colonization of _Malassezia_ species, abnormal sebum production, and altered immune response.
### Clinical Presentation:
- Erythematous, greasy or yellowish scales predominantly in seborrheic areas: scalp, nasolabial folds, eyebrows, ears, chest.
- Patients commonly report itchiness, irritation, and periodic flare-ups.
- May cause temporary, reversible hair shedding due to inflammation and follicular involvement (non-scarring alopecia).
### Diagnostic Approach:
- Primarily clinical diagnosis.
- Trichoscopy: greasy scales, erythema, perifollicular scaling, mild follicular inflammation.
- Biopsy rarely necessary; histology shows spongiosis, parakeratosis, superficial perivascular infiltrate, and yeast presence.
### Management:
- **First-line treatments:**
- Topical antifungals (ketoconazole shampoo/cream).
- Topical corticosteroids for short-term use (betamethasone lotion, hydrocortisone).
- **Maintenance:** Regular use of antifungal shampoos (zinc pyrithione, selenium sulfide, ketoconazole).
- **Adjunctive:** Anti-inflammatory and keratolytic shampoos (salicylic acid, coal tar shampoo).
---
## 2. Psoriasis of the Scalp
### Definition and Pathogenesis:
Chronic, immune-mediated inflammatory condition characterized by accelerated epidermal turnover and thickened plaques. Genetic predisposition and immunologic factors (T-cell dysregulation, TNF-alpha, IL-17) play critical roles.

### Clinical Presentation:
- Clearly demarcated, thick, silvery-white scaling plaques on erythematous bases, typically extending beyond hairline onto forehead, behind ears.
- Significant pruritus, discomfort, and social embarrassment.
- Hair loss typically due to manual removal of scales, trauma, or inflammation-induced telogen effluvium. Usually non-scarring.
### Diagnostic Approach:
- Clinical diagnosis usually sufficient.
- Trichoscopy: "red dots" (vascular loops), white scales, silvery-white plaques, absent follicular scarring.
- Biopsy if uncertain: hyperkeratosis, parakeratosis, Munro microabscesses, dilated capillaries in dermal papillae.
### Management:
- **Topical therapy:**
- Corticosteroids (clobetasol, betamethasone), vitamin D analogs (calcipotriene).
- Coal tar, salicylic acid shampoos.
- **Phototherapy:**
- Narrow-band UVB in severe or widespread cases.
- **Systemic therapy (severe cases):**
- Methotrexate, Cyclosporine, biologics (TNF-alpha inhibitors, IL-17 inhibitors).
- Patient education to avoid scalp trauma (Koebner phenomenon).
---
## 3. Fungal Infections (Tinea Capitis)
### Definition and Pathogenesis:
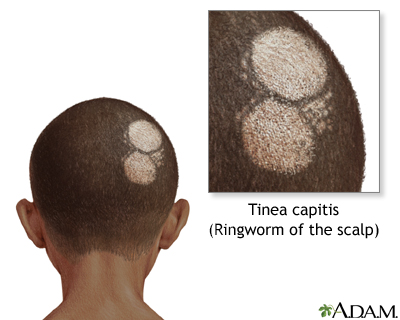
Tinea capitis is a dermatophyte fungal infection of the scalp and hair shafts, primarily affecting children but also seen in adults. Causative organisms: _Trichophyton tonsurans_, _Microsporum canis_, among others.
### Clinical Presentation:
- Patchy hair loss with broken hair shafts ("black dots").
- Scalp scaling, erythema, pustules, significant pruritus.
- Severe form (Kerion): intense inflammatory response, boggy swelling, pustules, pain, and potential scarring alopecia.
### Diagnostic Approach:
- Clinical suspicion confirmed by laboratory testing.
- **Trichoscopy:** corkscrew hairs, comma hairs, black dots, broken hairs.
- **Microscopy:** Potassium hydroxide (KOH) preparation reveals fungal hyphae.
- **Culture:** definitive species identification.
- Wood’s lamp: bright-green fluorescence (Microsporum species), but absent in Trichophyton species.
### Management:
- **First-line (systemic antifungals):**
- Oral Griseofulvin (first-line in children), Terbinafine (first-line in adults).
- Alternative: Fluconazole, Itraconazole.
- **Adjunctive therapy:** Antifungal shampoo (ketoconazole or selenium sulfide) to reduce infectivity.
- Management of Kerion: early initiation of systemic antifungals, short-term oral corticosteroids to prevent permanent scarring and hair loss.
---
## 4. Folliculitis and Eczema of the Scalp
### A. Folliculitis
#### Definition and Pathogenesis:
Inflammation or infection of hair follicles, often due to bacterial pathogens (_Staphylococcus aureus_) or irritation. Can lead to transient, non-scarring hair loss or permanent scarring alopecia (folliculitis decalvans) if chronic.
#### Clinical Presentation:
- Scattered follicular pustules, erythema, pruritus, tenderness.
- Severe forms (folliculitis decalvans): cicatricial alopecia, tufted hairs, scarring, and persistent inflammation.
#### Diagnostic Approach:
- Clinical exam: pustular lesions, erythema around follicles.
- Trichoscopy: pustules, crusts, tufted hairs (advanced folliculitis decalvans).
- Culture and sensitivity (in recurrent or severe cases) for targeted antibiotics.
- Biopsy (chronic or scarring cases): neutrophilic infiltrate around hair follicles, possible perifollicular fibrosis.
#### Management:
- Acute uncomplicated folliculitis: topical antiseptics or antibiotics (mupirocin, clindamycin solution).
- Recurrent/severe cases: oral antibiotics (doxycycline, clindamycin, rifampin combination).
- Folliculitis decalvans: prolonged oral antibiotic regimens, anti-inflammatory medications, adjunctive topical steroids.
### B. Scalp Eczema (Atopic and Contact Dermatitis)
#### Definition and Pathogenesis:
Chronic inflammatory skin disorder characterized by barrier dysfunction (atopic dermatitis) or exposure to irritants/allergens (contact dermatitis).
#### Clinical Presentation:
- Diffuse scalp erythema, dryness, scaling, intense pruritus, and scratching-induced hair loss (mechanical alopecia).
- Recurrent exacerbations and chronicity common.
#### Diagnostic Approach:
- Clinical: history of atopy, exposure to irritants/allergens (shampoos, dyes, hair products).
- Patch testing (if allergic contact dermatitis suspected).
- Trichoscopy: diffuse scaling, erythema, broken hairs secondary to scratching.
#### Management:
- Identify and eliminate irritants/allergens.
- Topical corticosteroids (moderate potency), topical calcineurin inhibitors (tacrolimus).
- Regular emollients, gentle shampoos, and barrier repair products.
- Systemic antihistamines for severe pruritus and preventing scratching-induced damage.
---
### Clinical Pearl:
- Many scalp conditions overlap in clinical presentation. Precise diagnosis using trichoscopy, careful history, targeted laboratory investigations, and biopsy when necessary is critical.
- Effective management of these disorders typically leads to significant improvement or complete recovery of associated hair loss.
This structured knowledge enables precision in diagnosis, tailored therapeutic approaches, and improved patient outcomes in managing scalp disorders associated with hair loss.