### Date : 2025-03-02 15:42
----
# **Chapter 2: Anatomy and Physiology of the Scalp**
## **2.1 Scalp Structure and Layers**
Understanding the **anatomy of the scalp** is crucial for performing **safe and effective Scalp Micropigmentation (SMP)**. The scalp consists of **multiple layers**, each with distinct properties that influence **pigment retention, healing, and long-term results**.
SMP practitioners must be able to **identify the correct layer** for pigment implantation to ensure **optimal color stability** and **prevent pigment migration or excessive fading**.
---
## **2.1.1 The Five Layers of the Scalp**
The scalp is composed of **five distinct layers**, remembered by the mnemonic:
**S** – Skin
**C** – Connective tissue (dense)
**A** – Aponeurosis (galea aponeurotica)
**L** – Loose connective tissue
**P** – Periosteum
These layers provide **structural support, vascular supply, and protective functions**.
---
### **1️⃣ Skin (Epidermis and Dermis) – The Target Layer for SMP**
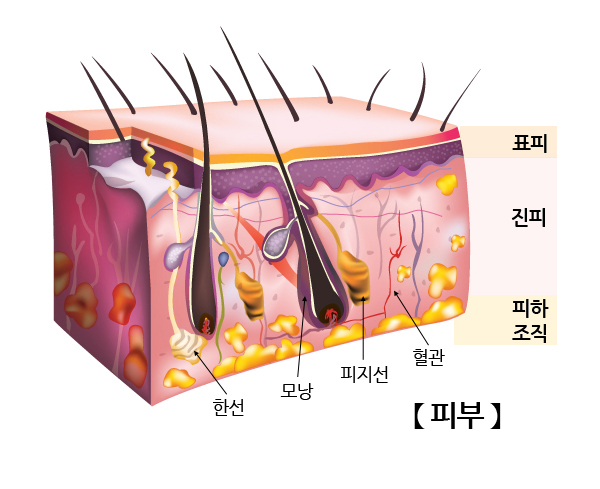
This is the **outermost layer** of the scalp, composed of the **epidermis and dermis**.
- The **epidermis** is the thin, outermost layer composed of **keratinized stratified squamous epithelium**. It has **no blood vessels** and receives nutrients via diffusion.
- The **dermis** is a **vascularized layer** containing **collagen, elastin, sebaceous glands, and hair follicles**.
#### **Implications for SMP**
- The **upper dermis** is the ideal depth for **pigment implantation**.
- If pigment is **placed too shallow** (epidermis only), it will **fade rapidly** due to continuous **cell turnover (desquamation)**.
- If pigment is **placed too deep** (mid-to-lower dermis), it can **spread or migrate**, leading to **blurred or unnatural-looking results**.
- SMP must be deposited at **0.5 to 1.5 mm depth** for **long-term stability**.
---
### **2️⃣ Connective Tissue Layer (Dense Fibrous Tissue)**
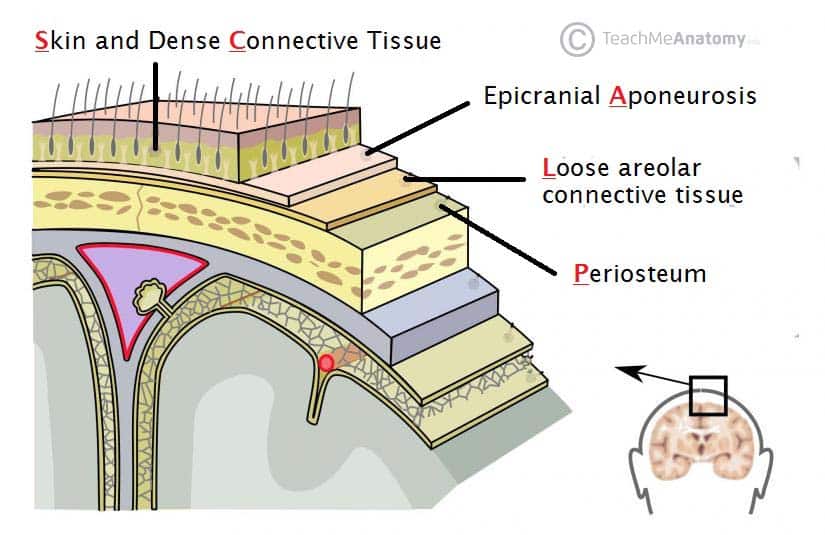
- This layer contains **a dense vascular network** and **fibrous septa that anchor the skin to the galea aponeurotica**.
- It houses **major blood vessels** and **nerve endings**, making it **highly sensitive**.
#### **Implications for SMP**
- **Bleeding is more likely** if SMP reaches this layer, as it contains **vascular plexuses**.
- Excessive pressure during SMP can cause **disruption of capillaries**, leading to **subdermal bleeding**, which can **alter pigment appearance**.
- **Proper needle depth control is essential** to avoid excessive vascular trauma.
---
### **3️⃣ Aponeurosis (Galea Aponeurotica)**
- A **tough fibrous layer** that **connects the frontalis and occipitalis muscles**.
- Functions as **a rigid, inelastic structure** that contributes to **scalp mobility**.
- This layer **lacks significant vascularization**, meaning it is relatively **avascular** compared to the surrounding layers.
#### **Implications for SMP**
- The **galea aponeurotica is not involved in SMP procedures**.
- In some cases, **SMP over scars** from trauma or surgery may involve the **galea**, requiring a **modified approach** to ensure pigment retention.
---
### **4️⃣ Loose Connective Tissue ("Danger Layer")**
- A **loose areolar layer** that allows **scalp movement**.
- Contains **emissary veins**, which can act as **conduits for infections** to spread into the **cranial cavity**.
#### **Implications for SMP**
- Pigment should **never** be deposited into this layer.
- Infections in this layer can lead to **serious complications**, including **deep scalp infections** or **abscess formation**.
- Practitioners must maintain **strict aseptic technique** to prevent contamination.
---
### **5️⃣ Periosteum (Bone Covering)**
- A **thin, vascular membrane** covering the **skull bones**.
- Contains **nerve endings**, making it **pain-sensitive**.
#### **Implications for SMP**
- **SMP pigment must not penetrate to this depth**.
- Over **bony prominences (e.g., vertex, frontal ridge), needle depth should be carefully adjusted** to avoid excess discomfort.
---
## **2.1.2 Scalp Vascularization and Blood Supply**
The scalp has a **rich vascular network** that plays a crucial role in **healing, pigment retention, and inflammation control**.
### **Major Arteries of the Scalp**
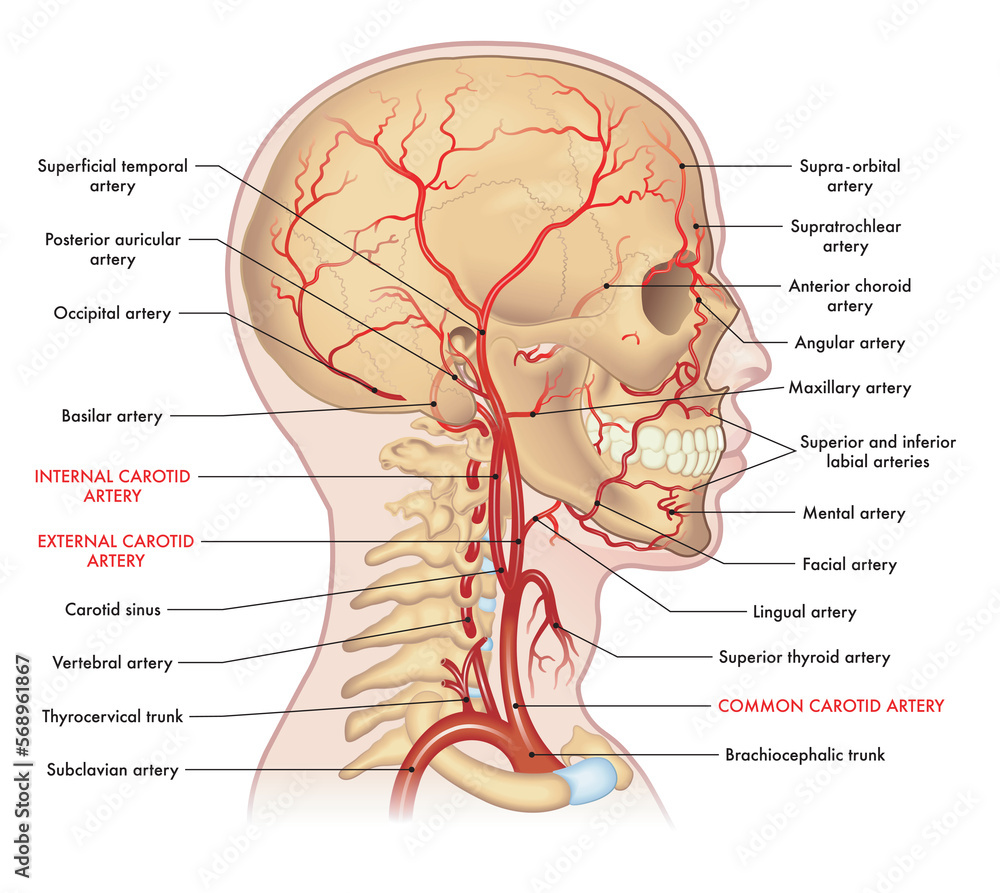
Blood supply to the scalp comes from the **external carotid artery** and **internal carotid artery**.
The five major scalp arteries include:

1. **Superficial Temporal Artery** – Supplies the lateral scalp and temples.
2. **Occipital Artery** – Supplies the posterior scalp.
3. **Posterior Auricular Artery** – Supplies the area behind the ears.
4. **Supratrochlear Artery** – Supplies the forehead and anterior scalp.
5. **Supraorbital Artery** – Also contributes to the anterior scalp blood supply.
#### **Implications for SMP**
- The **dense vascularization** of the scalp allows **rapid healing**, but **excessive bleeding can dilute pigment**, affecting retention.
- Proper **needle depth control** minimizes **capillary disruption** and ensures **optimal pigment absorption**.
- **Scalp edema (swelling) after SMP** is normal and usually resolves within 24–48 hours due to **high lymphatic drainage**.
---
## **2.1.3 Scalp Innervation and Sensory Distribution**
The scalp is highly innervated, which affects **pain perception during SMP**.
### **Major Nerves of the Scalp**
1. **Trigeminal Nerve Branches (CN V)**
- **Supratrochlear Nerve** (forehead sensation).
- **Supraorbital Nerve** (upper forehead and anterior scalp).
2. **Greater Occipital Nerve (C2)**
- Supplies sensation to the posterior scalp.
3. **Lesser Occipital Nerve (C2, C3)**
- Innervates the lateral scalp.
#### **Implications for SMP**
- **The most sensitive areas are the frontal hairline and crown**, where trigeminal and occipital nerve branches converge.
- Some patients may require **topical numbing agents** (lidocaine) to reduce discomfort during SMP.
- **Nerve damage is rare**, but improper SMP techniques (excess pressure, repeated trauma) may lead to **temporary numbness**.
---
## **2.1.4 Scalp Healing and Regeneration**
### **Normal Healing Process After SMP**
1. **Inflammatory Phase (0-3 Days)**
- Redness, mild swelling, and slight scabbing.
- Immune response begins clearing excess pigment particles.
2. **Proliferative Phase (3-14 Days)**
- Fibroblasts produce collagen.
- Scabs naturally shed, revealing **lighter, settled pigment**.
3. **Maturation Phase (2-6 Weeks)**
- Final pigment color stabilizes.
- Minor fading occurs (~30% of initial pigment).
#### **Factors Affecting Healing**
- **Skin Type** (Oily skin may fade faster).
- **Sun Exposure** (UV accelerates pigment breakdown).
- **Immune Response** (Stronger immune activity = faster fading).
- **Post-SMP Care Compliance** (Moisturization, avoiding excess sweating).
---
## **2.1.5 Conclusion**
Understanding the **layers of the scalp** is crucial for **precise SMP application**, minimizing complications, and achieving **long-lasting, natural results**.
- **The optimal pigment depth is in the upper dermis**, avoiding deeper structures.
- **Scalp vascularization and lymphatic drainage** influence **healing and pigment retention**.
- **Nerve innervation impacts patient pain perception**, and **proper technique ensures minimal discomfort**.
A strong **anatomical foundation** allows SMP practitioners to **tailor treatments based on individual scalp characteristics**, ensuring **consistent and natural-looking outcomes**.