### Date : 2025-03-04 15:17
----
# **2.2 Blood Supply and Innervation of the Scalp**
Understanding the **vascular supply and nerve innervation of the scalp** is essential for performing **safe and effective Scalp Micropigmentation (SMP)**. The **rich vascular network** of the scalp affects **healing, pigment retention, and the risk of excessive bleeding**, while the **complex nerve supply** influences **pain perception and patient comfort** during the procedure.
---
## **2.2.1 Blood Supply of the Scalp**
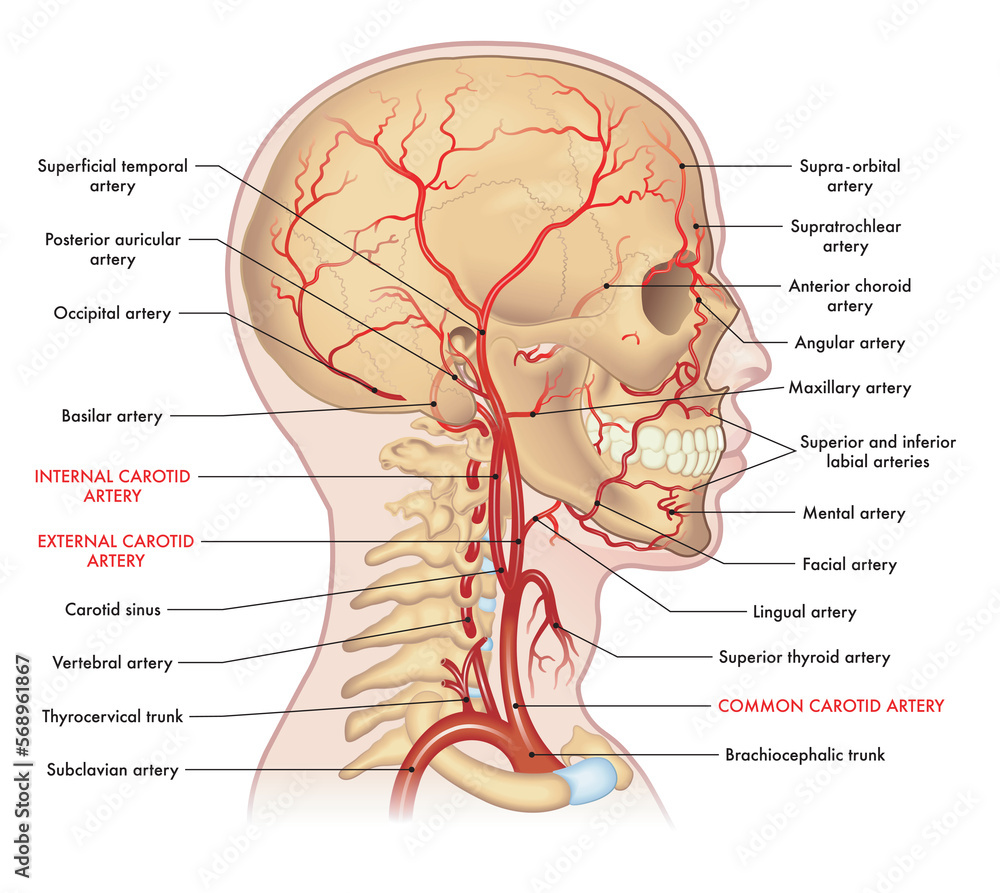
The scalp receives **dual arterial supply** from both the **external carotid artery** and **internal carotid artery**. These arterial networks form **anastomoses**, ensuring **a continuous blood supply**, even in cases of localized trauma or surgery.
### **A. Major Arteries of the Scalp**
The scalp’s arterial supply is derived from five major arteries:
### **1️⃣ Superficial Temporal Artery (Branch of External Carotid Artery)**
- Location: Courses **anterior to the ear** and ascends to supply the **lateral scalp** and **temporal region**.
- **Clinical significance**:
- This artery is often **palpable** in the **temple area**.
- Excessive SMP pressure in this region can cause **vascular trauma** leading to **localized swelling or bruising**.
- A major site for **botulinum toxin injections** for migraine treatment.
### **2️⃣ Occipital Artery (Branch of External Carotid Artery)**
- Location: Arises from the **posterior external carotid artery** and supplies the **back of the scalp**.
- **Clinical significance**:
- The **occipital region bleeds profusely** due to the **dense vascular network**.
- When performing **SMP for FUT/FUE scar camouflage**, avoiding deep penetration is essential to prevent **subdermal bleeding**.
### **3️⃣ Posterior Auricular Artery (Branch of External Carotid Artery)**
- Location: Courses behind the **ear** and supplies the **posterior-lateral scalp**.
- **Clinical significance**:
- Care must be taken in **post-auricular SMP applications** to prevent **vascular injury**, especially when working near **hair transplant scars**.
### **4️⃣ Supratrochlear Artery (Branch of Internal Carotid Artery)**
- Location: Supplies the **forehead and frontal scalp**.
- **Clinical significance**:
- The frontal scalp is **one of the most sensitive areas** due to both **vascular and nerve density**.
- SMP in this region should be performed with **controlled depth and pressure**.
### **5️⃣ Supraorbital Artery (Branch of Internal Carotid Artery)**
- Location: Extends from the **orbit** to supply the **upper forehead and anterior scalp**.
- **Clinical significance**:
- **High vascular density** in the forehead makes it **prone to bleeding**.
- SMP practitioners should use **lighter pressure** in this area to avoid excessive trauma.
---
## **2.2.2 Venous Drainage of the Scalp**

- The scalp’s veins **closely follow the arterial system** and drain into the **external and internal jugular veins**.
- The **danger zone** of the scalp is the **loose connective tissue layer**, which contains **emissary veins** that connect to **intracranial venous sinuses**.
- **Clinical significance**:
- **Infections of the scalp** can spread to the **brain via emissary veins**, leading to **[[Cavernous sinus thrombosis]]**, a life-threatening condition.
- Maintaining **strict aseptic technique** during SMP is critical to preventing **secondary infections**.
---
## **2.2.3 Innervation of the Scalp**
The scalp is richly innervated, making **pain perception a critical factor in SMP procedures**. The **nerves of the scalp** originate from two primary sources:
1. **Cranial Nerves (Trigeminal Nerve – CN V)**
2. **Cervical Nerve Roots (C2, C3)**
### **A. Sensory Nerves of the Scalp**
|**Nerve**|**Origin**|**Innervated Region**|**Clinical Significance**|
|---|---|---|---|
|**Supratrochlear Nerve**|Trigeminal (CN V1)|Medial forehead, anterior scalp|Very sensitive; anesthesia may be required for SMP.|
|**Supraorbital Nerve**|Trigeminal (CN V1)|Forehead, frontal scalp|Common site for botox injections.|
|**Zygomaticotemporal Nerve**|Trigeminal (CN V2)|Temporal scalp|Less commonly affected in SMP.|
|**Auriculotemporal Nerve**|Trigeminal (CN V3)|Lateral scalp, anterior to the ear|Can be irritated by repeated trauma.|
|**Greater Occipital Nerve**|C2|Posterior scalp|Compression can cause occipital neuralgia.|
|**Lesser Occipital Nerve**|C2, C3|Lateral-posterior scalp|Variably involved in posterior scalp sensation.|
---
## **2.2.4 Pain Perception in SMP Procedures**
Pain perception during SMP is highly variable, depending on **individual sensitivity**, **nerve distribution**, and **scalp hydration**.
### **A. Most Sensitive Areas for SMP**


- **Frontal hairline (Supratrochlear & Supraorbital nerves)**
- **Crown/Vertex (High nerve density from multiple branches)**
- **Temporal scalp (Auriculotemporal nerve)**
### **B. Least Sensitive Areas for SMP**
- **Occipital scalp (Less superficial nerve endings)**
- **Parietal region (Moderate innervation)**
### **C. Pain Management Strategies for SMP**
- **Topical Anesthetics**:
- **Lidocaine 5% cream** (applied 30 minutes before the procedure).
- **Epinephrine-containing anesthetics** (reduce bleeding).
- **Cooling Techniques**:
- Use of **cold compresses** before or after the procedure.
- **Needle Depth Control**:
- Ensuring pigment is deposited **only within the upper dermis** minimizes pain.
- **Session Planning**:
- Breaking sessions into **multiple shorter sittings** can reduce discomfort.
---
## **2.2.5 Clinical Implications of Scalp Vascularization and Innervation for SMP**
1. **Bleeding Control**
- The scalp is highly vascularized, meaning **SMP can induce pinpoint bleeding**.
- **Applying slight pressure with sterile gauze** during the procedure helps minimize bleeding.
2. **Pigment Retention**
- Excessive bleeding can cause **pigment dilution**, leading to **faster fading**.
- Patients should avoid **blood-thinning agents (aspirin, alcohol) before SMP**.
3. **Post-Procedure Healing**
- Due to **rich blood supply**, healing is **rapid**, and **scabs usually form within 24-48 hours**.
- Proper **post-procedure care**, including **moisturization and sun protection**, improves pigment retention.
4. **Pain Management**
- The **frontal scalp and vertex** are **more sensitive** due to trigeminal nerve branches.
- **Topical anesthetics** and **needle depth adjustment** help ensure a **comfortable procedure**.
---
## **2.2.6 Conclusion**
The **blood supply and nerve innervation of the scalp** directly impact **SMP technique, healing, and patient comfort**.
- **The scalp’s extensive vascular network** allows **rapid healing** but also **increases the risk of bleeding**.
- **Superficial nerve branches contribute to pain perception**, requiring **effective anesthesia and pain control strategies**.
- Proper **needle depth control, aseptic technique, and pigment application** are essential to **achieve natural-looking, long-lasting results**.